Root Causes of Overweight and Obesity: Community-Driven Solutions to Address Racial and Ethnic Disparities in RI

Providence, RI (June 6, 2023): Rhode Island KIDS COUNT will release its newest publication, Root Causes of Overweight and Obesity: Community-Driven Solutions to Address Racial and Ethnic Disparities in Rhode Island, on Wednesday, June 7, 2023, from 9:30 a.m. – 11:00 a.m. at Farm Fresh Rhode Island (10 Sims Avenue, Unit 103, Providence, RI 02909). Featured speakers will include Paige Clausius-Parks, Executive Director of Rhode Island KIDS COUNT, and Carolyn Belisle, Managing Director of Corporate Social Responsibility at Blue Cross & Blue Shield of RI. Highlights from the publication will be presented by Kaitlyn Rabb, Policy Analyst at Rhode Island KIDS COUNT. A conversation with community partners will include Michelle Rivera from Progreso Latino, Jesus Ayala Figueroa from South Providence HEZ/Family Service of RI, Liz Moreira from Pawtucket-Central Falls HEZ/LISC, and Belinda Phillipe of Central Providence HEZ/ONE Neighborhood Builders.
Developed with and for the Community
“Over the past six months, Rhode Island KIDS COUNT partnered with trusted community organizations to gather input on the root causes of childhood overweight and obesity in Central Falls, Pawtucket, and Providence,” said Kaitlyn Rabb, Policy Analyst at Rhode Island KIDS COUNT. “We held an in-person community conversation at Progreso Latino to gather input from Central Falls and Pawtucket parents and a virtual conversation to gather input from Providence youth and parents. These conversations allowed us to better understand the barriers families face and the community’s own recommendations for removing them.”
“The conditions and environments where children are born, live, learn, work, and play greatly impact their health outcomes,” said Paige Clausius-Parks, Executive Director of Rhode Island KIDS COUNT. “It’s unacceptable that in Rhode Island, Children of Color are less likely to have access to the conditions necessary for a healthy life. We must understand the root causes of disparities in children’s health outcomes and well-being and listen to the voices of the communities most impacted to create solutions that support the health of all children and youth. The community was clear on steps we must take, and the recommendations reflect the vision we see for a healthier future.”
Prevalence of overweight and obesity in Rhode Island children ages 2 – 17, 2021

- Prevalence of overweight and obesity in Rhode Island ages 2 to 17, 2021
- Core cities: 18% overweight, 32% obese
- Remainder of state: 15% overweight, 19% obese
- Rhode Island (overall): 16% overweight, 23% obese
- Half (50%) of Rhode Island children with no insurance/unknown insurance status are overweight or obese, compared to 47% of children with public insurance and 30% of children with private insurance.
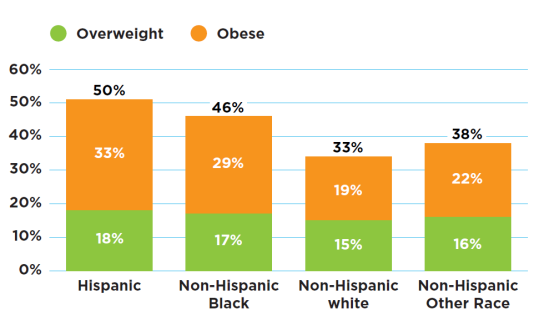
- In Rhode Island, Hispanic (50%) and Black (46%) children are more likely to be overweight or obese compared to white (33%) children.
- Since the onset of the COVID-19 pandemic, obesity rates for Black, Hispanic, other/multiple race, and white children have all increased. However, there are notable differences in overweight and obesity rates by race and ethnicity, with Black and Hispanic children continuing to have higher rates of overweight and obesity, and since the COVID-19 pandemic the disparities have widened.
-
- Low-income families and Families of Color were hit hardest by the COVID-19 pandemic and by the resulting economic crisis, and Children of Color were more likely to attend schools that were doing fully remote learning or to miss school due to COVID-19 or fears of exposure by their families, limiting access to healthy meals and opportunities for exercise at school. These factors are likely among the reasons why disparities widened.
An Important Note: The Limitations of BMI as a Measure of Children’s Health
- Although the Body Mass Index (BMI) it is currently the most widely used and accepted measure of population-level obesity and risk for adverse outcomes, it has limitations that contribute to misconceptions, biases, and inequities about weight and healthy living. The BMI measure does not factor in a person’s gender, sex, race, or ethnicity, which affects one’s weight and fat composition, and was created with measures on only white male adults.
- Reporting and interpreting data on weight (like BMIs) should be done within the context of population-level data that measure the underlying root causes of children’s health outcomes and well-being to better understand how and why children are overweight and how to support the health of all children and youth no matter where they live or the size of their body.
Social determinants of health
Structural factors (also referred to as social determinants of health or root causes) are important to understanding and addressing healthy weight and healthy living in childhood. Health care only accounts for 10-20% of an individual’s overall health outcomes and is just one of the social determinants of health, which is defined as the conditions and environments where people are born, live, learn, work, and play that greatly impact health outcomes. These social determinants of health, which account for over 80% of health outcomes, include:
- Food Access/Food Insecurity and Nutrition: affordability, food deserts, cultural competence.
- Food insecurity in childhood can lead to disruptions in eating patterns and habits that can contribute to poorer long-term health outcomes.
- Households of Color, low-income households, and households with children in Rhode Island were more likely to report being food insecure in 2022.
- Built Environment: green space, access to transportation, walkability of neighborhood, air pollution, noise pollution, safety.
- The walkability and safety of a neighborhood is another important factor that affects a child’s ability to be physically active and healthy. Low-income communities and Communities of Color are less likely to have access to green space to play in and this makes it difficult for children and families to be physically active. When there are green spaces in these communities, they are often of poorer quality and offer fewer amenities and opportunities for safe play than neighborhoods in higher-income communities.
- Air pollution (poor air quality) and noise pollution (unwanted or disturbing sound) are both key determinants of a built environment and limit access and opportunity for healthy habits and living conditions. The communities in Providence with the highest levels of noise are low-income communities and Communities of Color.
- Poverty/Socioeconomic Stress Factors and Barriers: depression, anxiety, trauma, lack of sleep.
- Children who live in poverty, especially those who experience deep poverty in early childhood, are more likely to have health, behavioral, educational, economic, and social problems and often lack access to healthy foods and recreational opportunities.
- Between 2017 and 2021, 15% of all Rhode Island children lived in poverty, 76% of whom were Children of Color. In 2020, more than half (59%) of Rhode Island’s Children of Color lived in one of the four core cities (Central Falls, Pawtucket, Providence, and Woonsocket, the cities with the highest child poverty rates), and more than three quarters of the children in Central Falls (90%) and Providence (85%) were Children of Color.
- Weight-stigma and Discrimination: bullying and marginalization, inaccessibility of environment.
- Weight-based societal discrimination is perpetuated by many in educational, workplace, health care, and community settings, perpetuating weight-based stigma rather than recognizing the complex root causes of overweight and obesity and the social determinants that are beyond an individual’s control.
Recommendations:
- Work with Communities of Color to identify needs that are rooted in and exacerbated by systemic racism and develop community-driven, racially aware solutions.
- Increase the accessibility of food banks and the quality and variety of food offered (culturally competent, nutritious, expand hours and capacity).
- Provide access to free healthy school meals to all Rhode Island children.
- Improve the quality of school meals. Provide opportunities for students to work with school vendors to sample and vote on healthy foods they would like to be included in school meal menus.
- Support partnerships between food pantries, farmers markets, community health workers, and schools to better support the nutrition needs of children with chronic or special needs.
- Promote collaboration between schools and parents to educate children on physical activity and nutrition.
- Improve the built environment in low-income communities by enacting intentional policies and providing urban planning resources that are equitable and mitigate the history of harm.
- Provide more accessible, affordable, and safe recreation spaces for children and families.
- Expand grant programs that could provide additional free or low-cost recreation activities for children and youth.
- Promote community collaborations (libraries, churches) to provide more engaging physical activity opportunities for children.
- Provide education and financial support to parents so they have the tools they need to provide nutritious foods and options for their children.
- Provide opportunities for parents to get more involved in advocacy opportunities.
- Improve the RI Works Program and increase Rhode Island’s Earned Income Tax Credit (EITC) to help Black, Latino, Asian, and Native American families meet their basic needs and move out of poverty.
- Provide opportunities for parents to get more involved in advocacy opportunities.
- Acknowledge and dismantle weight-based stigma and discrimination by creating weight-inclusive policies, protections, and spaces.